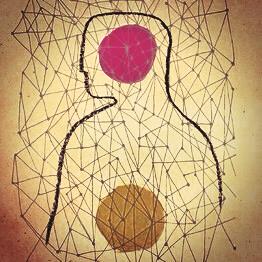
The Gut-Brain Connection
/The expressions, "gut-wrenching", "sick to my stomach", “gut reaction", “butterflies in stomach" are all commonly used in our culture for good reason. Simply, the gastrointestinal tract is sensitive to all emotion. Whether it’s anger, anxiety, sadness, excitement, or irritation; all of these feelings can trigger physical symptoms in the gut. Many times people describe it as a feeling of heaviness, tension, tightness, knotted or fluttering.
This Gut-Brain connection is bi-directional. A tense or stressed intestine sends signals to the brain, and visa verse, an overwhelmed brain sends signals to the gut. Hence, a person's stomach or intestinal distress can be the cause or the product of anxiety, stress, or depression. That's because the brain and the gastrointestinal (GI) system are intimately connected.
In recent years, neuroscientists have come to understand more clearly the powerful links between the human brain and gut bacteria. The vast variety of gut flora seems to have a major impact on our emotions and state of mind. The brain acts on gastrointestinal and immune functions that help to shape the gut's microbial makeup, and gut microbes make neuroactive biochemical compounds that also act on the brain. These complex interactions could occur in various ways: microbial compounds communicate via the vagus nerve, which connects the brain and the digestive tract, and microbially derived metabolites interact with the immune system, which maintains its own communication with the brain. With this information, scientists have been conducting studies with both probiotics and prebiotics to understand the effects on mood, particularly with anxiety and depression.
Researchers at Oxford University found that supplements designed to boost healthy bacteria in the gastrointestinal tract (“prebiotics”) may have an anti-anxiety effect insofar as they alter the way that people process emotional information. While probiotics consist of strains of good bacteria, prebiotics are carbohydrates that act as nourishment for those bacteria.
The results of one of the tests revealed that subjects who had taken the prebiotic paid less attention to negative information and more attention to positive information, compared to the placebo group, suggesting that the prebiotic group had less anxiety when confronted with negative stimuli. This effect is similar to that which has been observed among individuals who have taken antidepressants or anti-anxiety medication.
The researchers also found that the subjects who took the prebiotics had lower levels of cortisol — a stress hormone that has been linked with anxiety and depression — in their saliva when they woke up in the morning.
Mayer and his colleagues at UCLA uncovered the first evidence that probiotics ingested in food can be effective in reducing anxiety. The researchers gave healthy women yogurt twice a day for a month. Post-trial numbers indicated altered brain function in both a resting state and when performing an emotion-recognition task.
Stephen Collins, a gastroenterology researcher at McMaster University in Hamilton, Ontario, has found that two strains of bacteria, lactobacillus and bifidobacterium, reduce anxiety-like behavior in mice. And John Cryan, a neuroscientist at the University College of Cork in Ireland, has examined the effects of both of bifidobacterium microflora on depression in animals. In a 2010 paper published in Neuroscience, he gave mice either bifidobacterium or the antidepressant Lexapro; he then subjected them to a series of stressful situations, including a test which measured how long they continued to swim in a tank of water with no way out. After a short period of time, the mice were recovered and tested. It was found that the microbe and the drug were both effective at increasing the animals’ perseverance, and reducing levels of hormones linked to stress.
As scientists learn more about how the gut-brain microbial-neural network operates, there is great hope for a new frontier in treating psychiatric disorders, just as Prozac and other psychotropic medication is used today. The difference is that this method would be a natural alternative for eliminating the distressing and uncomfortable side-affects of these current medications. And most importantly, this method of treatment would address the causal factors that could lead to a “cure”, rather than just a reduction of symptoms that are seen in present day treatments.
-Tanya Vallianos
Tanya Vallianos, MA, LPC, ATR, NCC, EMDR III, EAP II is a psychotherapist in private practice in Fort Collins, CO. With a background in Naturopathic Medicine, she works from a holistic and integrated model that she believes is most helpful to her clients health and well-being. 970-420-9504